A retired York GP is heading off to Uganda for a whistlestop tour of six remote rural clinics to check on the progress of a pioneering medical experiment he helped set up.
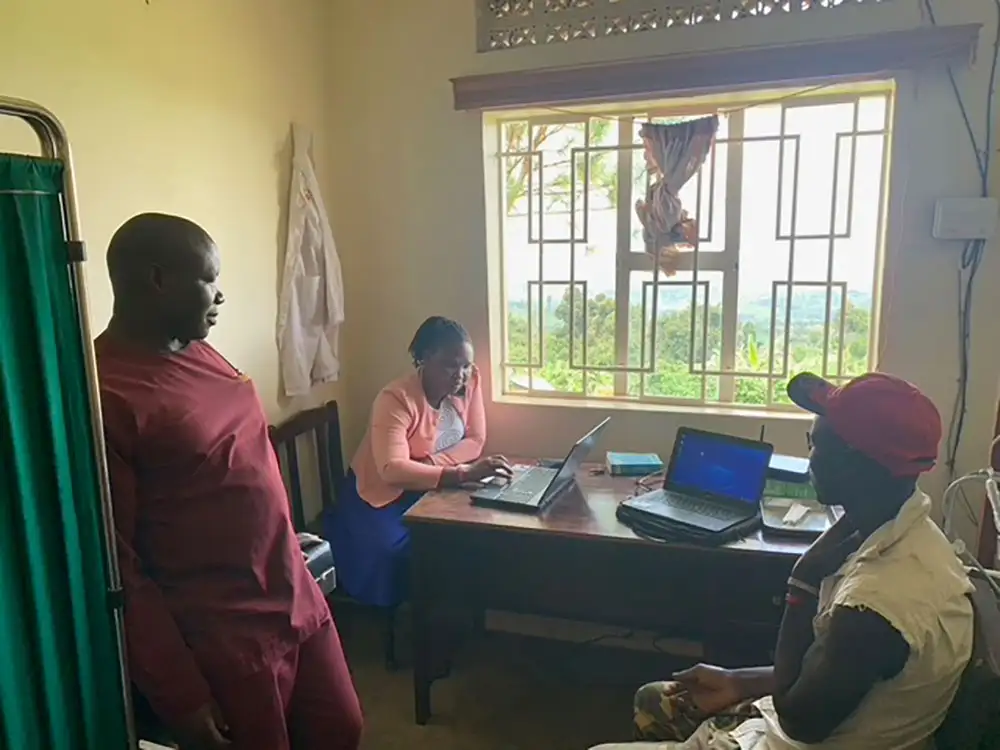
Peter Smith, 73, will be assessing the impact of a project to enable the clinics to keep electronic medical records for thousands of patients – and to submit those records directly to health bosses at Uganda’s health ministry.
It is a scheme that could enable rapid tracking of outbreaks of infectious diseases such as Ebola – potentially saving countless lives by stopping disease spreading.
At the moment, health agencies trying to keep track of diseases in remote areas of Uganda rely on handwritten medical records – records that can take weeks to be sent to the health ministry in Kampala and then weeks more to collate.
With the help of the ‘Project Connect’ electronic records system provided by Peter’s medical charity Outreach EMR, that can be done in hours rather than weeks.

“That makes a huge difference,” said Peter, who was a GP with the Haxby Medical Group for 30 years before he retired in 2012. “The quicker you recognise an outbreak and stop it spreading, the more lives can be saved.”
Peter set up Outreach EMR after retiring.
Thinking he still had something to offer, he spent nine weeks, at his own expense, working in a small medical clinic in the village of Bumwalukani in eastern Uganda.
It was a desperately poor area. Infant mortality was 15 times higher than in the UK, and there was no running water, no proper roads, no internet.
His clinic had a limited supply of basic medications – anti-malarials, antibiotics, rehydration pills for children with diarrhoea.
But Peter was seeing 90 children every day – and there was a problem. No one was keeping any medical records. It meant he was effectively treating children in the dark.
Peter didn’t know what drugs the children had already been given, whether there was medication they were allergic to – even how they’d contracted the conditions he was treating them for.
He began keeping his own handwritten records. But, when he went to use the local latrine, he found his notes had been torn up and recycled as loo paper. People in poor rural areas of Uganda recycle everything, he says.
Why electronic medical records?
It was a Eureka moment. Back in the UK, he teamed up with friend who was a software expert to design a simple electronic medical records system for laptop computers that, by using clever drop-down menus, would enable clinic staff with even basic literacy to keep a record of patients’ medical histories after just a few hours training.
Outreach EMR began in clinics in Uganda. Now, 11 years on, it is working in 23 clinics in nine of the poorest countries in the world, including Haiti, Nicaragua and the Philippines.
The charity, which is now run by a committee of 14 York volunteers, including Peter, is making a real impact, Peter says.
Lack of medical records contributes to up to 150,000 young mothers or newborn babies in Africa dying every year because they have missed vital checks that could have picked up pregnancy complications.

Up to a million people in Africa die every year, meanwhile, because of simple medical errors like prescribing the wrong drugs – errors that could be prevented with medical records.
Peter estimates Outreach EMR saves about 250 lives a year in the 23 clinics where it operates. “And if we were in more clinics, we could save more lives,” he said.
Which is where his visit to Uganda on October 4 comes in.
The project he is monitoring is a pilot set up with the support of the Uganda government.
As well as enabling local clinics to keep their own medical records, it enables them to quickly summarise records and regularly send reports to the Ministry of Health in Kampala. This enables the quick tracking of outbreaks of disease.
Outreach EMR has even provided solar panels at one clinic, so they have electricity to enable the data to be sent over the internet using mobile phones.
But the pilot project is just the beginning.

While he’s in Uganda, Peter will visit officials at the Ugandan Ministry of Health. He hopes to persuade them to allow Outreach EMR to roll out its system to hundreds more clinics in remote areas of Uganda.
“We have the capacity for up to 300 more clinics,” he said.
Imagine how many lives could be saved if that happens…
- Outreach EMR needs to raise £100,000 a year to keep going. To find out more about the charity, or make a donation, visit Electronic Medical Records for Primary Care | Outreach EMR | Global